What to Expect: From Your First IVF Consult to Your Egg Retrieval
Infertility is defined as the inability to get or stay pregnant after a full year of actively trying. Once an unspoken diagnosis, infertility has become a socially acceptable topic and is more common than many people might think. In fact, it's estimated that infertility affects over 186 million (1 in 8) people across the world.
Everything you need to know before IVF
A diagnosis of infertility can produce a range of emotions and can be both complex and overwhelming. For many people, IVF (in vitro fertilization) is the best option for achieving a healthy pregnancy. As an embryologist, I have found that many people enter IVF treatment with very little guidance. This article provides a detailed description of what to expect from the time you enter a fertility clinic for your initial consult through your egg retrieval.
Note: I am not a doctor. Please always discuss any health concerns with your doctor before making any decisions about your health.
Step 1: The Initial Consult
Before your doctor can determine the best course of treatment, your fertility doctor will review your (and your partner's, if applicable) medical history. Some people already know their diagnoses prior to their initial consult (from a gynecologist or urologist, for example), while others do not know their cause of infertility. Your doctor may perform an ultrasound to observe your reproductive organs and will likely order diagnostic tests, which may include some of the following:
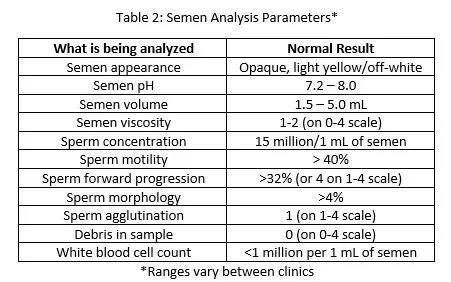
Baseline hormone levels: these blood tests determine your hormone levels without IVF stimulation. Your doctor may test your E2 (estradiol), FSH (follicle-stimulating hormone), LH (luteinizing hormone), TSH (thyroid stimulating hormone), T4 (testosterone), and/or P4 (progesterone) levels. Each clinic will have their own reference ranges for each of these hormones, and these ranges will differ depending on what day of your menstrual cycle you are on when the blood is drawn.
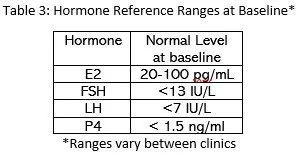
2. AMH (anti-Mullerian hormone): this blood test helps predict a woman's ovarian reserve (how many eggs she has remaining in her ovaries). Women are born with all of the eggs that they will ever have, and these numbers naturally decreases as women age). In general, a lower AMH level correlates to a lower ovarian reserve, while a higher AMH level correlates to a higher ovarian reserve. However, an AMH level is not a definitive method for determining a woman's chance of success, and it is typically one of multiple diagnostic tests performed prior to an IVF cycle. Though each clinic has their own parameters, see Table 1 for average AMH level reference ranges.
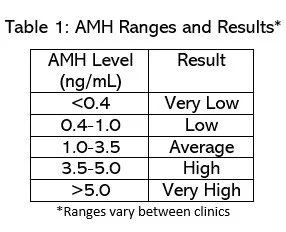
3. Semen analysis (if not already performed): this procedure analyzes both the semen (fluid portion) and sperm in an ejaculate. Though some clinics perform different tests, and each clinic has their own parameters, see Table 2 for some common semen analysis tests and reference ranges. Your doctor may recommend having multiple semen analyses performed since sperm parameters can change over time.
4. Carrier screening: this blood test determines if either parent (or donor) is affected by or a carrier of any genetic mutations that can be passed down to their embryo(s). Examples of these mutations include cystic fibrosis and sickle cell anemia.
5. Hysterosalpingogram (HSG): this procedure involves injecting a contrast media (dye) into the uterus and then examining the pathway of the media using an x-ray. This procedure can determine if the uterus is abnormally shaped and if either of the Fallopian tubes are blocked.
6. Sonohysterogram (sono): this procedure involves injecting saline into the uterus and examining the uterine lining for polyps, fibroids, and/or scarring using an ultrasound.
7. Hysteroscopy: this procedure involves inserting a small camera into the uterus to examine the uterine lining for polyps, fibroids, and/or scarring.
8. Antral follicle count (AFC): this test is typically performed using a transvaginal ultrasound at the beginning of your menstrual cycle. Your doctor will examine and count how many eggs have begun to grow at the beginning of the menstrual cycle. Each menstrual cycle, multiple follicles begin to grow as the eggs inside of them mature. However, (usually) only one egg ultimately ends up growing while the others degenerate. The antral follicle count can help your doctor estimate how many eggs will be retrieved and how many eggs are remaining in the ovaries. Again, this test is not definitive.
Once some or all of these tests have been performed, your doctor can determine your best course of treatment (ovulation induction, IUI, IVF, etc.). For the purpose of this article, we will assume that your doctor has determined that IVF is your best treatment option. So, what happens next?
The timing of your IVF cycle correlates with the timing of your menstrual cycle. Some doctors will prescribe birth control pills prior to an IVF cycle, which helps prime the body for the IVF cycle.
Baseline Monitoring Appointment
You should contact your clinic on the first day of your period. Your clinic will likely schedule a baseline monitoring appointment ~2 days later. During this appointment, two events will occur:
A transvaginal ultrasound: this shows how many antral follicles (small follicles that begin to grow at the beginning of every menstrual cycle) are in your ovaries, which can help predict how many eggs will mature during your IVF cycle. The baseline ultrasound also checks for any large ovarian cysts and/or other abnormalities that may interfere with the IVF process, and it confirms that the uterine lining is thin (as it should be when menstruation occurs).
Blood tests: these tests confirm that you are not pregnant and record your FSH, LH, E2, and P4 levels. Though each clinic has their own reference ranges, see Table 3 for average baseline hormone levels.
If everything looks good on your baseline testing, you will begin taking IVF medications, known as gonadotropins, which will hyper-stimulate your ovaries so multiple follicles (with eggs inside of them) grow.
Monitoring Appointments
Most clinics will have you return 3-5 days later for your next monitoring appointment. This appointment will consist of the following monitoring:
A transvaginal ultrasound: this shows the number and size of the follicles inside the ovaries. At this point, you should expect to see multiple follicles (this number may be less than your AFC) in each ovary that have grown in size since your baseline scan. At this point, the diameter of your follicles can be measured in millimeters using the ultrasound.
A blood test that measures your blood hormone levels.
Medication + Monitoring Appointments
If your hormone levels look appropriate and your follicles seem to be growing, you will typically begin taking a medication to prevent premature ovulation (your eggs cannot be retrieved if ovulation occurs too early), and you will return to the clinic in 2-5 days (this varies between patients/clinics) for another monitoring appointment. This monitoring appointment will consist of the following:
A transvaginal ultrasound: this shows the number and size of the follicles inside the ovaries. At this point, you should expect to see around the same number of follicles that were seen at your previous ultrasound (sometimes less since not all follicles respond to the medications), but they should be larger than they were at your previous ultrasound.
A blood test that measures your blood hormone levels.
Again, your follicle sizes are measured in millimeters. Typically, follicles under ~16mm are too small to house mature eggs. Follicles can grow ~1-3mm per day depending on how your body responds to the IVF medications, so the next few days may consist of daily trips to the IVF clinic for monitoring.
The dosage of your IVF medications may be altered to ensure that you have the best stimulation possible. Keep in mind that the quality of the eggs outweighs the number of eggs that are retrieved, so it is important to let them mature at the perfect pace.
Over the next few day(s), you will continue the same type of monitoring until two events occur:
Some or all of your follicles are the "perfect size" (the protocol varies between clinics, but a typical "perfect size" is roughly 18-22mm).
Your E2 level is roughly 500-3500 pg./mL (~200 pg./mL per mature egg).
At this point, you should be ready for your ovulation trigger. Administering this medication essentially causes an LH surge to occur, which then triggers ovulation to occur. Your trigger medication must be administered exactly when directed (typically 35-36 hours prior to your egg retrieval time), which should occur right before ovulation. If ovulation occurs before the egg retrieval, the eggs can become "lost" and un-retrievable.
My name is Jessica and I am the voice behind Explaining IVF. I obtained my Master of Biomedical Science at Colorado State University and have been an embryologist since 2018. My favorite part of being an embryologist is helping people build their families. I started Explaining IVF to educate people about IVF and infertility so they can make informed decisions about their treatments and optimize their results. In my free time, I enjoy traveling, reading, and spending time with my friends and family.
Website: www.ExplainingIVF.com
Medical Disclaimer:
The information provided in this blog is intended for general informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your healthcare provider or qualified medical professional with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this blog.
References:
1. How Common is Infertility? (cnyfertility.com)
2. All About Sperm (explainingivf.com)
3. What's a Good AMH at Every Age? (natalist.com)
4. Fertility Testing Without Needles at Boston IVF
6. Fertility Hormone Levels and Sperm Parameters - Monitoring at Home (fairhavenhealth.com)