What Is a Mosaic Embryo?
What is mosaicism?
Whether you have personally undergone IVF or learned about it, you’ve probably heard the term “mosaic embryo.” While this term is relatively new, it’s become a widely-discussed and highly-debated topic in the IVF community since its implementation as a genetic classification in 2015. With all of the new studies regarding mosaic embryos constantly emerging, it’s important to understand what makes an embryo mosaic and why mosaicism matters. Let’s break this all down based on our current knowledge of mosaic embryos.
Background Information
Let’s first talk about embryos and their genetics. Sperm and egg cells both contain one set of genetic material, known as DNA, which is wound up into 23 structures known as chromosomes. This means that these cells contain half the amount of DNA of any other cell in the human body. When a sperm cell fertilizes an egg cell, their DNA combines to form a fertilized egg (zygote) that has two sets of DNA (one set from the sperm and one set from the egg).
From this point forward, the zygote will begin its own cell division (mitosis), dividing from one cell to two cells, and then to four cells, and so on. Each cell replicates (makes a copy of) its DNA before each cell division, and the DNA should evenly disperse into the original cell and the new cell. Thus, you end up with two cells with exactly the same DNA (and, again, one set of this DNA is from the sperm and one set is from the egg). So, in theory, every single cell in an embryo, fetus, and even an adult should have exactly the same DNA.
But that’s in a perfect world, and it’s actually not as common as you might think. In reality, it’s possible for sperm, egg, embryonic, fetal, and adult cells to have an abnormal amount of DNA in their cells. Some of these abnormalities are not harmful, while others can be lethal.
How Does Mosaicism Occur?
It begins with the sperm and the egg. These cells undergo two cell divisions (this is known as meiosis, and it’s how these cells end up with only one set of DNA instead of two). During these cell divisions, it’s possible for some of the DNA (part of a chromosome, a whole chromosome, or multiple chromosomes) to not evenly disperse into the cells. As a result, the sperm cell that fertilizes an egg may have the wrong amount of DNA, and/or the egg cell that is fertilized may have the wrong amount of DNA. When this occurs, the zygote gets the wrong amount of DNA, and this wrong DNA is replicated and passed on to each cell in the embryo. These embryos are known as aneuploid, or genetically abnormal, since their cells contain the incorrect amount of DNA.
Mosaicism is a little different because it results from errors in cell division after fertilization has occurred. As a result, the embryo ends up with two different cell lines (cells with different DNA). This arises one of two possible ways:
The sperm and/or egg had the incorrect amount of DNA, so the zygote also had the wrong amount of DNA. But the embryo’s cells began to correct the error at some point during early cell division. As a result, some of the embryo’s cells have the wrong number of DNA (from before the correction), while some have the correct number of DNA (from after the correction).
More commonly, the sperm and egg had the correct amount of DNA, so the zygote also had the correct amount of DNA. But at some point in early cell division, an error occurred that resulted in an uneven disbursement (nondisjunction) of DNA between the original and new cell. The result is two cells with different amounts of DNA, which both go on to divide and create more cells with different amounts of DNA.
An embryo’s chromosomes can be detected through preimplantation genetic testing (PGT) during in vitro fertilization (IVF) prior to embryo implantation. Additionally, amniocentesis, chorionic villus sampling, and other possible screening techniques can be performed after implantation has occurred. PGT is normally performed 5-7 days after fertilization occurs in the IVF laboratory.
What does PGT tell us?
PGT is performed through an embryo biopsy, during which 5-10 cells are removed from the embryo with microscopic tools and a laser. Embryos are not typically harmed during this process and are frozen (stored in liquid nitrogen) directly after the biopsy occurs. The biopsied cells are transported to a genetic testing company, which analyzes the DNA in those cells and determines how many of the cells in each biopsy sample have the correct number of chromosomes (i.e. the right amount of DNA).
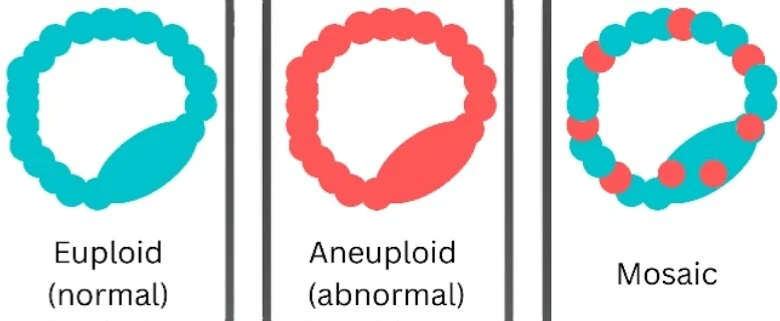
The results of PGT are determined based on the percentage of cells in the biopsy sample that have the correct amount of DNA. Though each company may have its own parameters, the results generally appear as:
Euploid (normal): 0-20% of the cells in the sample have the wrong amount of DNA
Mosaic: 20-80% of the cells in the sample have the wrong amount of DNA
Aneuploid (abnormal): 80-100% of the cells in the sample have the wrong amount of DNA
As you can see, there is a 60% range for mosaic embryos. Since this range is so wide, many genetic testing companies categorize mosaic embryos according to the percentage of abnormal cells. One common categorization includes:
Low mosaic: 20-40% of the cells in the sample have the wrong amount of DNA
Moderate mosaic: 40-60% of the cells in the sample have the wrong amount of DNA
High mosaic: 60-80% of the cells in the sample have the wrong amount of DNA
Can Mosaic Embryos be Transferred?
There is still a lot of debate surrounding the transfer of mosaic embryos, but there seems to be a common conclusion: the higher the level of mosaicism (i.e. the more abnormal cells), the lower the chances of success.
Though the studies are still new and limited, one study of 18 mosaic embryos found that these embryos can lead to healthy births, and mosaic embryos that went to term had a normal karyotype (had the right number of chromosomes). Another study involving 137 mosaic embryos found that mosaic embryos can result in healthy live births, but they have higher miscarriage rates and lower live birth rates compared to genetically normal embryos. Finally, a 2021 study compared the transfers of euploid, low mosaic, and moderate mosaic (<50%) embryos and found no significant difference in their live birth rates and neonatal outcomes. Further, there was no mosaicism detected in the pregnancies or newborns. Other relevant studies can be found here.
Overall, these studies all prove hopeful for those with mosaic embryos available for transfer. It’s important to keep in mind that only 5-10 cells are being biopsied from an embryo that should have nearly 150 total cells. Further, the cells that are biopsied are trophectoderm cells, which ultimately develop into the placenta. You may wonder why we don’t biopsy the cells that ultimately develop into the baby (the inner cell mass, or ICM). The theory is that all portions of the embryo should have a population of cells with the same DNA as the other portions, so taking a biopsy from any portion of the embryo should represent the genetic makeup of the entire embryo. So, we choose to take cells from the trophectoderm to avoid damaging the ICM.
Is it possible that the results of the biopsy sample do not actually represent the genetic makeup of the entire embryo? It’s possible. But we have to remember that this is all new technology that is constantly advancing.
Final Notes
We also have to remember that there are different types of genetic abnormalities. Some abnormalities are harmless, while others can be lethal. For these reasons, it’s still advised that you speak with a genetic counselor before transferring a mosaic embryo to determine the risks involved with the transfer.
If you have undergone PGT and have a mosaic embryo (or more) in storage that you are considering transferring, I recommend joining mosaic embryo support groups. These include My Perfect Mosaic Embryo and Mosaic Embryo Discussion and Support on Facebook, though many more exist. I also recommend keeping up with the research regarding mosaic embryos and speaking with a genetic counselor if you have any questions regarding your mosaic embryos.
My name is Jessica and I am the voice behind Explaining IVF. I obtained my Master of Biomedical Science at Colorado State University and have been an embryologist since 2018. My favorite part of being an embryologist is helping people build their families. I started Explaining IVF to educate people about IVF and infertility so they can make informed decisions about their treatments and optimize their results. In my free time, I enjoy traveling, reading, and spending time with my friends and family.
Website: www.ExplainingIVF.com
Medical Disclaimer:
The information provided in this blog is intended for general informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your healthcare provider or qualified medical professional with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this blog.